Transient Ischemic Attack (TIA): Your Urgent Call To Action
In the complex network of our body's systems, the brain stands as the command center, orchestrating every thought, movement, and sensation. Its optimal functioning relies on a constant, uninterrupted supply of oxygen-rich blood. However, sometimes this vital flow can be briefly disrupted, leading to a condition known as a Transient Ischemic Attack, or TIA. Often referred to as a "mini-stroke," a TIA is far more than just a fleeting moment of discomfort; it's a critical warning sign, a loud alarm bell signaling the potential for a more severe event: a full-blown stroke.
Understanding what a TIA is, how to recognize its symptoms, and the immediate steps to take is paramount for anyone, regardless of age. While the phrase "tia kemp young" might bring to mind a specific individual or a demographic, the underlying medical reality of a TIA is universal. It underscores the urgent need for awareness and prompt medical intervention to prevent potentially life-altering consequences. This comprehensive guide will delve into the intricacies of TIAs, emphasizing why they are medical emergencies that demand immediate attention, and how timely action can be the key to safeguarding your future health.
Table of Contents
- What is a Transient Ischemic Attack (TIA)?
- TIA vs. Stroke: Understanding the Crucial Differences
- Recognizing the Warning Signs: Symptoms of a TIA
- The Urgent Need for Action: Why a TIA is a Medical Emergency
- TIA in Focus: Addressing Risk Factors and Prevention
- Life After TIA: Managing Long-Term Health
- Aphasia and TIA: A Potential Connection?
- Safeguarding Your Future: The Preventative Power of TIA Awareness
What is a Transient Ischemic Attack (TIA)?
A Transient Ischemic Attack (TIA) is a short period of symptoms strikingly similar to those of a stroke. The fundamental cause is a brief blockage of blood flow to the brain. Unlike a full stroke, where the blockage leads to permanent brain damage, a TIA's symptoms resolve completely and quickly, typically lasting less than five minutes, and almost always less than an hour. The clot responsible for this temporary obstruction usually dissolves on its own or gets dislodged before it can cause lasting harm to brain cells. However, this doesn't diminish its seriousness. Having a TIA often means you could have a stroke in the very near future. It's a critical indicator that something is amiss with your cerebrovascular health, making it a medical emergency you absolutely shouldn’t ignore.
- Ice In Spanish
- Shannen Doherty Death
- Light Skin Monkey
- Calendario Chino De Embarazo 2024
- Madelyn Cline Feet
The human body relies on a constant supply of oxygen delivered by blood to every cell, especially those in the brain. If this blood flow gets blocked, even temporarily, it can lead to neurological deficits. While a TIA doesn't cause permanent brain damage, it serves as a powerful opportunity to get treatment that can prevent a future, more devastating stroke. This concept is vital for everyone to grasp, from the general public to medical professionals, emphasizing the proactive steps needed after experiencing such an event.
TIA vs. Stroke: Understanding the Crucial Differences
While the symptoms of a TIA are identical to those of an ischemic stroke, their impact on the brain differs significantly. The key distinction lies in the outcome: TIAs do not cause permanent brain damage. This means that after a TIA, the blockage breaks up quickly and dissolves on its own, and brain tissue does not die. In contrast, an ischemic stroke results in the death of brain cells due due to prolonged lack of blood flow, leading to lasting neurological deficits. This crucial difference is why TIAs are often referred to as "mini-strokes" – they are a warning, not a full-blown attack with permanent consequences, yet. Infarction, or tissue death, is very unlikely if deficits resolve within one hour.
Despite this difference, the immediate response to TIA symptoms must be the same as for a stroke. The reason is simple: medical professionals cannot immediately tell whether a patient is experiencing a TIA or a full stroke. Both present with sudden, similar symptoms. Therefore, every TIA should be treated as an urgent medical emergency, demanding immediate evaluation. This urgency is particularly critical because approximately one in three people who experience a TIA will eventually have a stroke, with about half of these occurring within a short period after the TIA. Recognizing a TIA and having the cause identified and treated can significantly help prevent a future stroke, making it a pivotal moment for intervention.
Recognizing the Warning Signs: Symptoms of a TIA
The symptoms of a TIA are sudden and mirror those of a stroke, but their transient nature is what sets them apart. They happen abruptly and can include a range of neurological impairments. It's crucial for everyone, including young individuals, to be aware of these signs. For instance, if you consider a hypothetical scenario involving "tia kemp young" or any young person, recognizing these symptoms immediately could be life-saving.
Common symptoms of a TIA include:
- Numbness or weakness: Especially on one side of the body, affecting the face, arm, or leg. This sudden unilateral weakness is a hallmark sign.
- Difficulty speaking or understanding speech (aphasia): Slurred speech, inability to form words, or trouble comprehending what others are saying.
- Vision problems: Sudden blurring, dimming, or loss of vision in one or both eyes, often described as a "curtain coming down."
- Sudden, severe headache: With no known cause.
- Loss of balance or coordination: Dizziness, vertigo, or trouble walking, especially when combined with other symptoms.
- Confusion: Sudden disorientation or difficulty thinking clearly.
Since the symptoms of TIA and stroke are identical, if you experience any of these symptoms, even if they disappear quickly, seek medical attention right away. Do not wait for them to pass or assume they are insignificant. Every second counts in evaluating and potentially preventing a major stroke.
The Urgent Need for Action: Why a TIA is a Medical Emergency
A TIA is not just a warning; it's an urgent call to action. The transient nature of the symptoms can be misleading, making some individuals dismiss them as minor or temporary. However, ignoring a TIA is a grave mistake. It signifies an underlying problem with blood flow to the brain that, if left unaddressed, could lead to a permanent stroke. A prompt evaluation of your symptoms is vital not only to diagnose the cause of a transient ischemic attack but also to allow your healthcare professional to determine the best course of treatment to prevent a future stroke. This is where the principles of E-E-A-T (Expertise, Authoritativeness, Trustworthiness) and YMYL (Your Money or Your Life) are critically important; timely, expert medical intervention is paramount.
The Underlying Causes of TIA
The loss of blood flow to an area of the brain that causes a TIA can be attributed to several factors, primarily related to blockages in the arteries. These include:
- A blood clot in an artery of the brain: This is often due to atherosclerosis, a condition where plaque builds up in the arteries, narrowing them and making them prone to clot formation.
- A blood clot that travels to the brain from somewhere else in the body: For example, a clot could originate in the heart (due to conditions like atrial fibrillation) and travel up to the brain, lodging in a smaller artery.
- Narrowing of a blood vessel in the brain: Severe stenosis (narrowing) of the carotid artery in the neck, which supplies blood to the brain, is a common cause.
Identifying the specific cause is crucial for effective prevention strategies. This is why a thorough medical investigation is always necessary after a TIA.
Diagnostic Tools: Uncovering the Root Cause
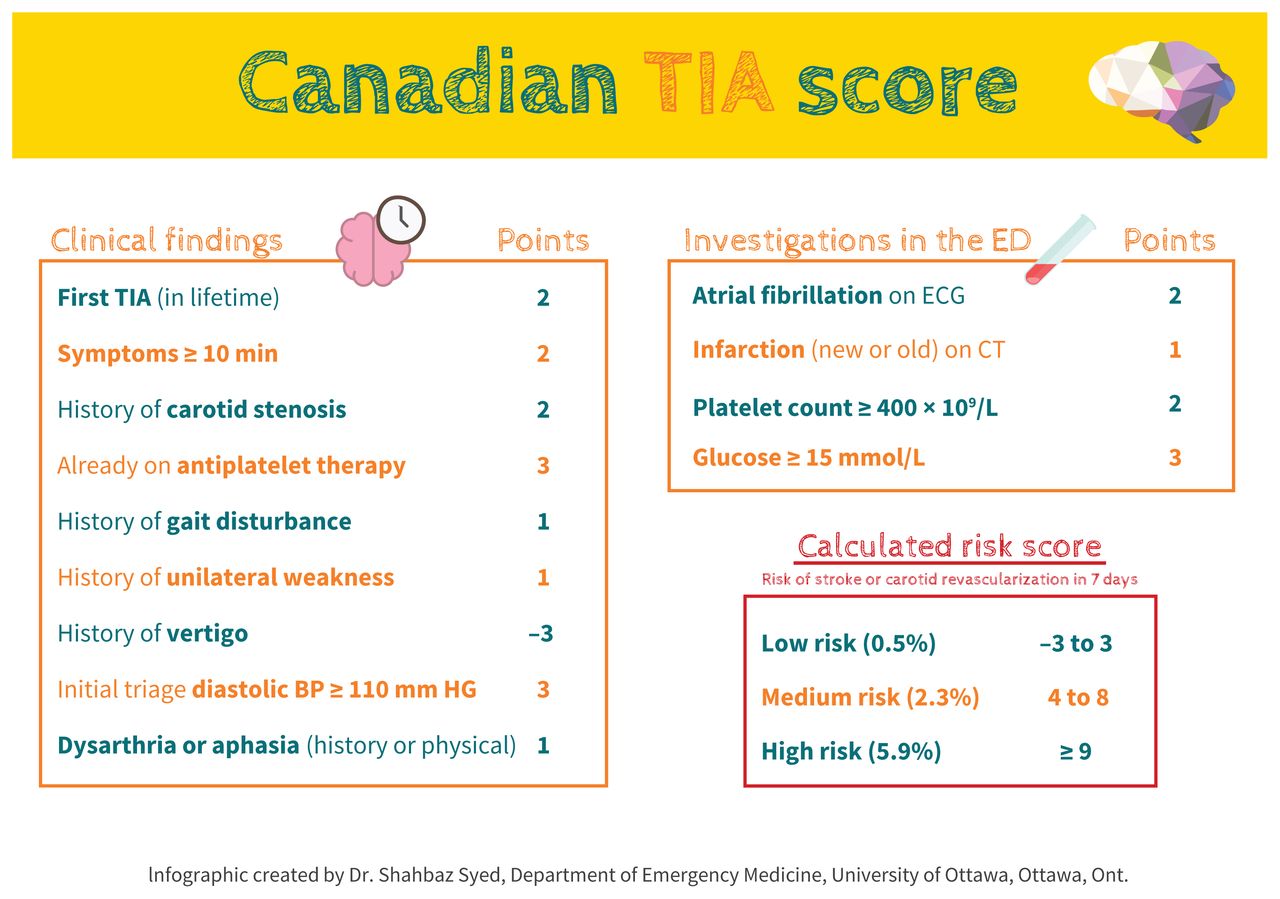
To pinpoint the cause of the TIA and to assess your risk of a stroke, your healthcare professional may rely on a range of diagnostic tests. These tests help visualize the brain, blood vessels, and heart to identify any abnormalities. Common diagnostic tools include:
- Magnetic Resonance Imaging (MRI): This imaging technique uses powerful magnets and radio waves to create detailed images of the brain, helping to detect any areas of damage or abnormalities in blood vessels.
- Computerized Tomography (CT) Scan: A CT scan uses X-rays to create cross-sectional images of the brain, which can quickly identify bleeding or signs of stroke.
- Carotid Ultrasound: This test uses sound waves to create images of the carotid arteries in the neck, checking for narrowing or plaque buildup.
- Echocardiogram: An ultrasound of the heart to check for blood clots or other heart conditions that could lead to a stroke.
- Blood Tests: To check for risk factors like high cholesterol, diabetes, or clotting disorders.
These tests provide critical information that guides the treatment plan, ensuring that the underlying cause of the TIA is addressed to prevent future, more severe events. The speed and accuracy of these diagnostics are paramount in the immediate aftermath of a TIA.
TIA in Focus: Addressing Risk Factors and Prevention
The primary goal after a TIA is to prevent a future stroke. This involves a multi-faceted approach that addresses underlying risk factors and may include lifestyle changes, medications, and sometimes surgical interventions. Understanding and managing these aspects is crucial for long-term health, particularly for individuals who might be at a higher risk, or even for younger individuals, such as in a "tia kemp young" scenario, where early intervention can significantly alter their health trajectory.
Targeted Treatments for TIA Prevention
Treatment strategies for TIA are highly individualized, based on the identified cause and the patient's overall health. Common approaches include:
- Lifestyle Changes: These are foundational and include maintaining a healthy diet, regular exercise, quitting smoking, limiting alcohol intake, and managing stress.
- Medications:
- Antiplatelet drugs: Such as aspirin or clopidogrel, are often prescribed to prevent blood clots from forming.
- Anticoagulants: For individuals with conditions like atrial fibrillation, blood thinners may be prescribed to prevent clots from forming in the heart and traveling to the brain.
- Cholesterol-lowering drugs (statins): To reduce plaque buildup in arteries.
- Blood pressure medications: To manage hypertension, a major risk factor for stroke.
- Cilostazol: If the cause of the TIA is narrowing of blood vessels in the head, cilostazol might be recommended in conjunction with aspirin or clopidogrel.
- Ticagrelor (Brilinta) and Aspirin combination: Healthcare providers might prescribe a 30-day course of ticagrelor combined with aspirin to reduce the risk of recurrent stroke, especially in the immediate period after a TIA.
- Surgery: In cases of severe carotid artery disease, where the main artery supplying blood to the brain is significantly narrowed, surgery (carotid endarterectomy) may be recommended to remove plaque and restore blood flow.
These interventions are designed to reduce the risk of future blockages and ensure adequate blood flow to the brain, thereby preventing a debilitating stroke.
The Role of Specialized Care in TIA Management
Given the complexity of cerebrovascular conditions, specialized care is often essential for effective TIA management. Institutions like Mayo Clinic exemplify a multidisciplinary approach, bringing together experts from various fields to provide comprehensive care. Their teams include:
- Cerebrovascular neurologists: Doctors trained in blood vessel and brain conditions.
- Endovascular surgical neuroradiologists: Specialists in blood vessel conditions and imaging.
- Vascular neurosurgeons: Experts in blood vessel conditions and brain surgery.
- Physical medicine and rehabilitation specialists: For recovery and long-term management.
- Emergency medicine professionals: For immediate assessment and stabilization.
- And other areas, ensuring a holistic approach to patient care.
This collaborative model ensures that patients receive quality care and have the best chance for successful recovery and stroke prevention. Such integrated care is crucial for addressing all facets of a TIA, from immediate diagnosis to long-term preventative strategies.
Life After TIA: Managing Long-Term Health
Experiencing a TIA is a wake-up call that necessitates a commitment to long-term health management. While the symptoms of a TIA resolve, the underlying risk factors for stroke remain. Therefore, ongoing monitoring and adherence to treatment plans are crucial. This includes regular follow-ups with healthcare providers, consistent medication adherence, and continued dedication to a healthy lifestyle. For individuals like "tia kemp young" or any person who has had a TIA, this ongoing vigilance is key to preventing a future, more severe cerebrovascular event. It’s about empowering individuals with the knowledge and tools to actively participate in their health journey.
Managing conditions such as high blood pressure, diabetes, and high cholesterol becomes even more critical. Patients are often advised to monitor their blood pressure at home, maintain a balanced diet rich in fruits and vegetables, engage in regular physical activity, and avoid smoking. Education about recurrent stroke symptoms is also vital, ensuring that individuals and their families know when to seek emergency care again.
Aphasia and TIA: A Potential Connection?
Aphasia is a disorder that affects how you communicate. It can impact your speech, as well as the way you write and understand both spoken and written language. Aphasia usually happens suddenly after a stroke or a head injury, where brain damage occurs in the language centers. The severity of aphasia depends on the extent and location of the brain damage.
Given that TIA symptoms are similar to stroke symptoms, aphasia can indeed be a transient symptom of a TIA. If a TIA affects the language-processing areas of the brain, a person might experience temporary difficulty speaking or understanding. The crucial difference, as with other TIA symptoms, is that these communication difficulties resolve completely and quickly, typically within minutes. If aphasia persists, it suggests a stroke rather than a TIA, indicating permanent brain damage. Therefore, the presence of even temporary aphasia during a TIA underscores the urgency of medical evaluation, as it points to a disruption of blood flow in a critical area of the brain.
Safeguarding Your Future: The Preventative Power of TIA Awareness
In conclusion, a Transient Ischemic Attack (TIA) is a powerful and often underestimated warning sign. It is a temporary shortage of blood flow to the brain, but its implications are anything but temporary. While it doesn't cause permanent damage, it dramatically increases the risk of a future stroke, a potentially devastating event that can lead to long-term disability or even death. The phrase "tia kemp young" serves as a reminder that these events can affect anyone, regardless of age, making universal awareness paramount.
Recognizing the sudden onset of TIA symptoms—such as numbness, weakness on one side, vision problems, or difficulty with speech—and acting immediately by seeking emergency medical attention is the most critical step. A TIA is a medical emergency that offers a unique window of opportunity for intervention. Through prompt diagnosis, identification of the underlying cause, and aggressive treatment, the risk of a subsequent, more severe stroke can be significantly reduced. This proactive approach not only saves lives but also preserves quality of life. Be informed, be vigilant, and never ignore the warning signs. Your future health may depend on it.
If you or someone you know experiences symptoms of a TIA, do not hesitate. Call emergency services immediately. Early detection and treatment are your best defense against stroke. For more information on cerebrovascular health, consider consulting reputable medical resources.
- Merry Chrysler
- Hard Fought Hallelujah Lyrics
- Help I Accidentally
- Tini Mac And Cheese
- Happy Ending Near Me
Transient ischemic attack and minor stroke: diagnosis, risk

What Is a TIA (Transient Ischemic Attack) and How Can It Affect Vision?

Transient Ischemic Attack (TIA) - YouTube